Many clinical scenarios, especially those involving critically ill or injured patients, rely on single or serial Hb measurement determinations for clinical decision making.
Frequent laboratory testing and oversampling are factors that can lead to phlebotomy-related blood loss and development of anemia in the hospital setting.
Could one drop of blood and a second be enough for the answers you need?
![]() Lab-accurate results in less than 1 second
Lab-accurate results in less than 1 second
![]() Flexible measurement options using Hb or Hct values
Flexible measurement options using Hb or Hct values
![]() Intuitive symbols instead of error codes
Intuitive symbols instead of error codes
![]() Flexible connectivity options using Bluetooth or USB cable
Flexible connectivity options using Bluetooth or USB cable
![]() Large memory capacity up to 4000 results
Large memory capacity up to 4000 results

 Designed for challenging climate conditions
Designed for challenging climate conditions
![]() Flexible power supply options
Flexible power supply options
![]() Cleaned with a common cotton swab
Cleaned with a common cotton swab
![]() Microcuvette holder designed to prevent accumulation of dirt and residue
Microcuvette holder designed to prevent accumulation of dirt and residue
Whether detecting anemia or internal bleeding in a busy emergency department, monitoring a patient in the intensive care unit, or tending to a geriatric patient in outpatient setting, healthcare providers can benefit from access to immediate lab-accurate results at the patient bedside.
HemoCue® Hb 801 System in hospital setting only for markets where EU IVDD CE mark is applicable.
One important parameter measured, is hemoglobin (Hb) concentrations to identify anemia pre-, peri- and post-operative. Evidence suggest that anemia in hospitalized patients contributes not only to poor outcomes in chronically ill patients1, increases mortality, morbidity rates and length of stay (LOS), but also increases cost of health care delivery2.
Pre-operative anemia due to iron deficiency is common (30-40%) and is associated with increased rates of blood transfusion and increased morbidity after surgery4. It should be detected and treated prior to elective surgery5.
![]() POC Hb testing can be an effective strategy in the surgeon's office to screen for anemia in advance of surgery to allow adequate time for treatment intervention.
POC Hb testing can be an effective strategy in the surgeon's office to screen for anemia in advance of surgery to allow adequate time for treatment intervention.
Measurement of Hb is a critical part of blood transfusion decisions in the peri-operative period. In reality, it can take 30-45 minutes to get the Hb results of a stat sample returned from the laboratory6.
![]() Rapid measurement of POC Hb testing can help optimize transfusion support7.
Rapid measurement of POC Hb testing can help optimize transfusion support7.
Post-operative anemia may be present in up to 80-90% of patients undergoing major surgery8. Blood loss after surgery can continue through drains or in traumatized tissue, or due to repeated phlebotomy during prolonged port-operative hospitalization.
![]() During recovery from major surgery, Hb should be monitored on a regular daily basis, at least until 3rd post-operative day8.
During recovery from major surgery, Hb should be monitored on a regular daily basis, at least until 3rd post-operative day8.
The HemoCue® Hb 801 System was designed to support you in your daily work with maintaining point-of-care testing (POCT) analyzers, performing quality controls and training operators.
Help your staff to understand and leverage the full capacity and usage of Hb 801 with easy installation and training support from HemoCue.
Quality products, responsive on-site training and comprehensive training offering from HemoCue deliver value over the long-term and help you meet your needs for training and compliance.
 The HemoCue® Hb 801 System was designed to provide an intuitive workflow that can be easily operated by both medical and non-laboratory personnel. Factory calibrated against the ICSH recommended reference method; no further calibration needed.
The HemoCue® Hb 801 System was designed to provide an intuitive workflow that can be easily operated by both medical and non-laboratory personnel. Factory calibrated against the ICSH recommended reference method; no further calibration needed.
 The HemoCue® Hb 801 System is robust, can be cleaned with common cotton swabs and the unique microcuvette holder design prevents accumulation of dirt and residues.
The HemoCue® Hb 801 System is robust, can be cleaned with common cotton swabs and the unique microcuvette holder design prevents accumulation of dirt and residues.
 With intuitive symbols and animations, large display and simple operational steps, the HemoCue® Hb 801 System requires minimum training.
With intuitive symbols and animations, large display and simple operational steps, the HemoCue® Hb 801 System requires minimum training.
In our Knowledge Center, you will find useful videos, webinars, White Papers, scientific content and much more.
The HemoCue® Hb 801 System is based on the Hb/HbO2 isosbestic point at 506 nm and compensation for turbidity at 880 nm.
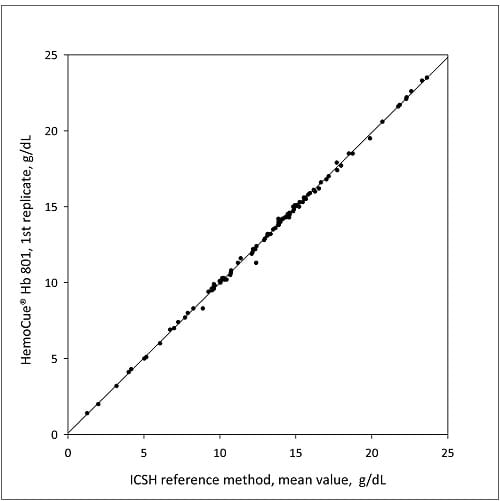
All HemoCue Hb systems are factory calibrated against the hemiglobincyanid method (HiCN), which is the international reference method recommended by ICSH (International Council for Standardization in Heamatology) for hemoglobin concentration in blood, and no further calibration is required.
Performance comparison conducted between the Hb 801, Hb 201+ and Hb 301 show that the systems are comparable. No clinical differences are noted between the systems and they all demonstrated excellent correlation against the HiCN reference method.
The ability to verify proper functioning of a system is an integral part of point-of-care testing. The HemoCue® Hb 801 System has an internal quality control, a self-test, that verifies that the optical parts of the analyzer are working properly.
The self-test, which is indicated on the analyzer display, is performed automatically each time the analyzer is turned on, when the cuvette holder is put back into place after removal, and every hour when in use. The self-test checks the linearity of the optronic unit by monitoring the current through the diodes and measuring the output current on the detector.
If external quality control is required by local or other regulations, controls recommended by HemoCue should be used.
1) Krishnasivam et al. Anemia in hospitalized patients: an overlooked risk in medical care. Transfusion 2018;58;2522–2528
2) Lawrence Tim Goodnough et al. Anemia and its Clinical Consequences in Patients with Chronic Diseases. The American Journal of Medicine, Volume 116 (7A).
3) Nedra S. Whitehead, et al. Interventions to prevent iatrogenic anemia: a Laboratory Medicine Best Practices systematic review. Critical Care (2019) 23:278.
4) Nicole R. Guinn et al. How do we develop and implement a preoperative anemia clinic designed to improve perioperative outcomes and reduce cost? Transfusion. 2016 Feb;56(2):297-30.
5) Susana Gómez-Ramirez, et al. Perioperative anemia: Prevalence, consequences and pathophysiology. Transfusion and Apheresis Science, Volume 58, Issue 4 August 2019, Pages 369-374.
6) Nataraj Madagondapalli Srinivasan et al. Intra-operative point of care haemoglobin estimation: A comparison of three methods. Sri Lankan Journal of Anesthesiology 18(1):15 -19 (2010).
7) Giancarlo Maria Liumbruno et al. Recommendations for the transfusion management of patients in the peri-operative period. II. The intra-operative period. Blood Transfusion 2011;9:189-217.
8) M. Munoz et al. An international consensus statement on the management of postoperative anemia after major surgical procedures. Anesthesia 2019, 73(11):1418-1431.

